University Hospitals Medicare Advantage Plan by PTHP
Quality
Top-rated Medicare Advantage service
Our plan has the best rating you can get.
5 out of a possible 5 stars!
Get 5-star treatment with our plan. For 2024, the Centers for Medicare and Medicaid Services (CMS) awarded PrimeTime Health Plan its highest rating of 5-stars.
How does it work?
- Medicare gets information from member satisfaction surveys, plans and health care providers.
- Medicare scores how well plans perform in several categories, including quality of care and customer service.
- Each fall, Medicare gives overall performance ratings between 1 and 5 stars based on that information.
- Star Ratings are released annually and reflect the experiences of people enrolled in Medicare Advantage plans.
- A 5-star rating is considered excellent.
- The Star Ratings system supports the Centers for Medicare and Medicaid Services efforts to empower people to make healthcare decisions that are best for them.
- These ratings help you compare plans based on quality and performance.
- You can switch from your current Medicare plan to one with a “5-star” quality rating during what’s called a Special Enrollment Period.
- You may do this only once and between December 8 and November 30.
- As CMS puts it, “More stars mean a better plan — for example, members may get better care and better, faster customer service.”
Our mission is to lead our community to improved health. We are committing to providing you with a superior level of customer service and access to quality care. To achieve our goal, we continually monitor and evaluate our performance against rigorous national and regional standards. To do this, we utilize data from HEDIS® and CAHPS® every year.
What is HEDIS® and CAHPS®?
HEDIS® is the Healthcare Effectiveness Data and Information Set. Insurance companies across the United States participate in HEDIS® data collection making it one of the best ways to gauge our performance against benchmarks. This data set includes over 90 measures that evaluate six different domains, including:
o Effectiveness of Care
o Access/Availability of Care
o Experience of Care
o Utilization and Risk-Adjusted Utilization
o Health Plan Descriptive Information
o Measures Collected Using Electronic Clinical Data System
CAHPS® is the Consumer Assessment of Healthcare Providers and Systems. This set of surveys asks patients to report on their healthcare experiences with both their health plan and their providers. This data is collected annually and plays a key role in how we strive to improve year after year.
HEDIS® is the Healthcare Effectiveness Data and Information Set. Insurance companies across the United States participate in HEDIS® data collection making it one of the best ways to gauge our performance against benchmarks. This data set includes over 90 measures that evaluate six different domains, including:
o Effectiveness of Care
o Access/Availability of Care
o Experience of Care
o Utilization and Risk-Adjusted Utilization
o Health Plan Descriptive Information
o Measures Collected Using Electronic Clinical Data System
CAHPS® is the Consumer Assessment of Healthcare Providers and Systems. This set of surveys asks patients to report on their healthcare experiences with both their health plan and their providers. This data is collected annually and plays a key role in how we strive to improve year after year.
UNDERSTANDING THE RESULTS
Below you can find the description and the questions associated with each table listed below.
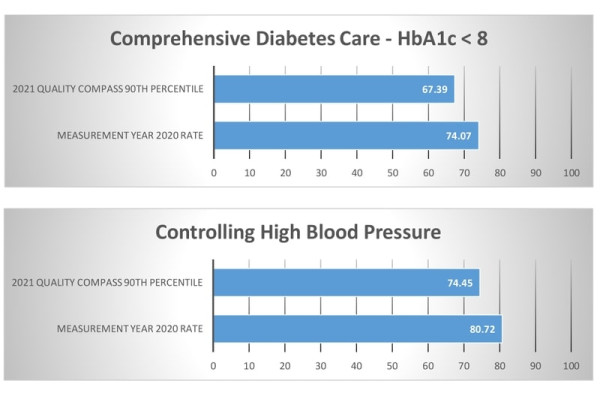
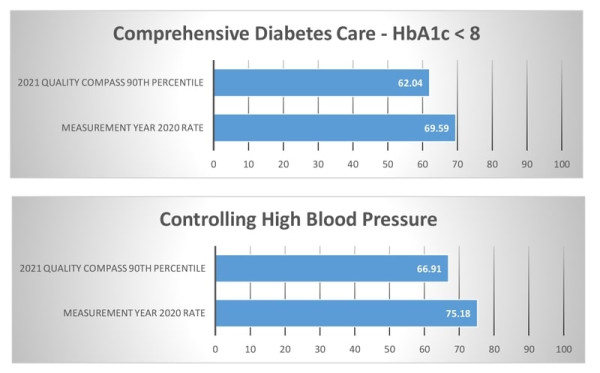
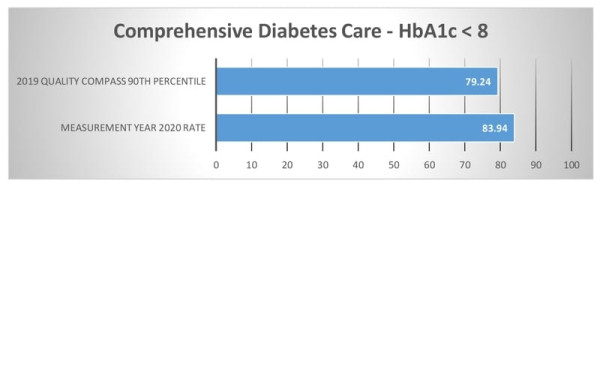
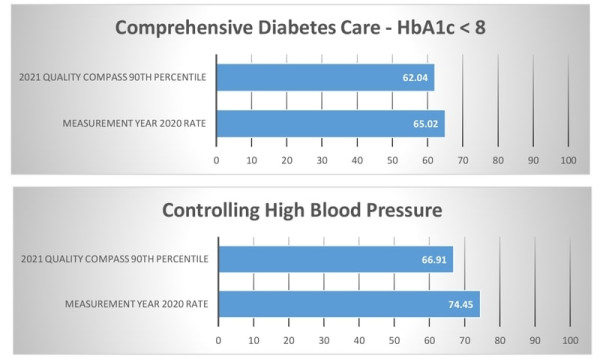
| Comprehensive Diabetes Control The percentage of members ages 18 to 75 years with diabetes who had HbA1c testing. |
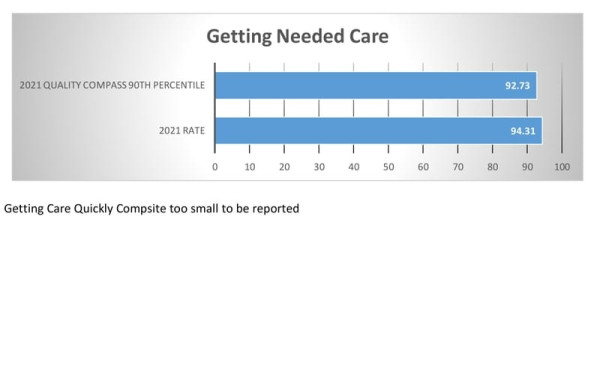
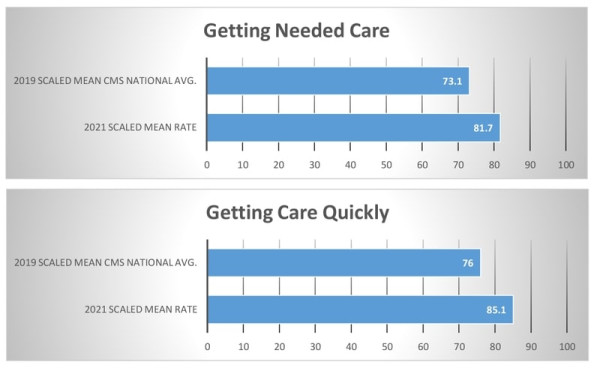
Getting Needed Care How often was it easy to get the care, tests, or treatment you needed? How often did you get an appointment to see a specialist as soon as you needed? |
| Controlling High Blood Pressure The percentage of members ages 18 to 85 years who had a diagnosis of hypertension and whose blood pressure was adequately controlled, less than 140/90. |
Getting Care Quickly When you needed care right away, how often did you get care as soon as you needed? How often did you get an appointment for a check-up or routine care at a doctor’s office or clinic as soon as you needed? |
The following HEDIS data represents the measurement year 2020 and reporting the year 2021. The following CAHPS data represents the measurement year 2021.
HOW WE COMPARE AGAINST OTHER PLANS
HMO
|
HEDIS®
 |
CAHPS®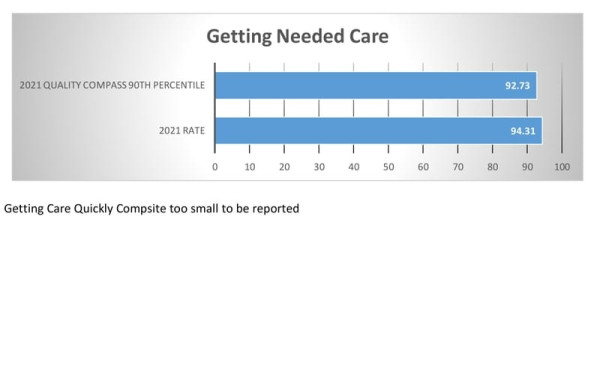 |
PPO
|
HEDIS®
 |
CAHPS®
 |
PrimeTime Health Plan
|
HEDIS®
 |
CAHPS®
 |
MARKETPLACE (QHP)
|
HEDIS®
 |
CAHPS®
 |
Disclaimers:
The source for certain health plan measure rates and benchmark (averages and percentiles) data (“the Data”) is Quality Compass® 2021 (Commercial) and 2019 (Medicare) and is used with the permission of the National Committee for Quality Assurance (“NCQA”). Any analysis, interpretation or conclusion based on the Data is solely that of the authors, and NCQA specifically disclaims responsibility for any such analysis, interpretation or conclusion. Quality Compass is a registered trademark of NCQA.
The Data comprises audited performance rates and associated benchmarks for Healthcare Effectiveness Data and Information Set measures (“HEDIS®”) and HEDIS CAHPS® survey measure results. HEDIS measures and specifications were developed by and are owned by NCQA. HEDIS measures and specifications are not clinical guidelines and do not establish standards of medical care.
NCQA makes no representations, warranties or endorsement about the quality of any organization or clinician who uses or reports performance measures, or any data or rates calculated using HEDIS measures and specifications, and NCQA has no liability to anyone who relies on such measures or specifications.
NCQA holds copyright in Quality Compass and the Data and may rescind or alter the Data at any time. The Data may not be modified by anyone other than NCQA. Anyone desiring to use or reproduce the Data without modification for an internal, noncommercial purpose may do so without obtaining approval from NCQA.
All other uses, including commercial use and/or external reproduction, distribution, or publication, must be approved by NCQA and are subject to a license at the discretion of NCQA. ©2021 & 2019 National Committee for Quality Assurance, all rights reserved.
The source for certain health plan measure rates and benchmark (averages and percentiles) data (“the Data”) is Quality Compass® 2021 (Commercial) and 2019 (Medicare) and is used with the permission of the National Committee for Quality Assurance (“NCQA”). Any analysis, interpretation or conclusion based on the Data is solely that of the authors, and NCQA specifically disclaims responsibility for any such analysis, interpretation or conclusion. Quality Compass is a registered trademark of NCQA.
The Data comprises audited performance rates and associated benchmarks for Healthcare Effectiveness Data and Information Set measures (“HEDIS®”) and HEDIS CAHPS® survey measure results. HEDIS measures and specifications were developed by and are owned by NCQA. HEDIS measures and specifications are not clinical guidelines and do not establish standards of medical care.
NCQA makes no representations, warranties or endorsement about the quality of any organization or clinician who uses or reports performance measures, or any data or rates calculated using HEDIS measures and specifications, and NCQA has no liability to anyone who relies on such measures or specifications.
NCQA holds copyright in Quality Compass and the Data and may rescind or alter the Data at any time. The Data may not be modified by anyone other than NCQA. Anyone desiring to use or reproduce the Data without modification for an internal, noncommercial purpose may do so without obtaining approval from NCQA.
All other uses, including commercial use and/or external reproduction, distribution, or publication, must be approved by NCQA and are subject to a license at the discretion of NCQA. ©2021 & 2019 National Committee for Quality Assurance, all rights reserved.
CAHPS is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ).”

Learn More from Our Local Specialists.
We are here to help you.
- Call us at 216-535-4014 | 1-833-954-0483 | (TTY 711)* from 8 a.m. to 8 p.m., Monday through Friday. Talk to a local specialist or schedule a 1-on-1 meeting to discuss your options.

Trisha
216-535-4014

Debbie
216-535-4014

Karen
216-535-4014